Background: Diagnosing multiple myeloma (MM) is challenging, because MM can present with a myriad of non-specific signs and symptoms, such as bone pain, fatigue, fractures, infection, within an elderly patient population (median age of MM diagnosis is 70 years). Patients with MM therefore experience significant delays in diagnosis, resulting in increased morbidity and reduced survival. In the primary care setting, the presence of bone pain in combination with laboratory abnormalities, such as hypercalcaemia or unexplained renal impairment, have a critical diagnostic role in MM. However, the occurrence of these clinical features prior to MM diagnosis within a population-based incident cohort of patients with MM has not been previously well described.
Aims: To describe the frequency and timing of the initial clinical features among patients with newly diagnosed MM (NDMM) in the UK primary care setting.
Methods: We used Clinical Practice Research Datalink (CPRD), an electronic health records database, derived from routinely collected general practitioner (GP) data across the UK primary care, containing approximately 17.1 million patients at the time of analysis. We identified patients with NDMM (2006-2016), aged ≥18 years with no history of solid tumors, and ≥2 years of GP registration prior to MM diagnosis. Baseline clinical characteristics were assessed during the 2-year period before MM diagnosis. We assessed clinical features, including bone pain, skeletal-related events (SREs) and CRAB criteria (hyperCalcemia, Renal failure, Anemia, Bone lesions) for MM during the 2-year period before MM diagnosis and from the time of symptom presentation or relevant diagnostic CRAB criteria to the diagnosis of MM.
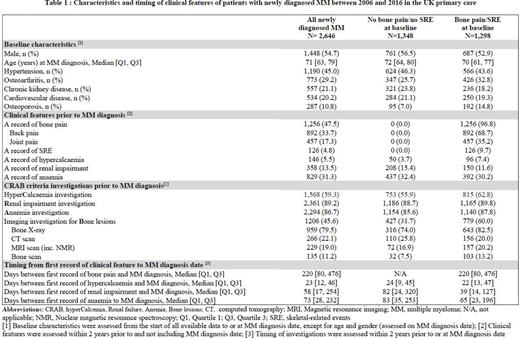
Results: We identified 2,646 eligible patients with NDMM with a median [Q1, Q3] age of 70 [61, 77]; 53.3% of patients were male. During the 2-year period prior to MM diagnosis, 47.5% of patients had a record of bone pain, mainly affecting the back or other joints, and 4.8% had a record of SRE. The median time between the first record of bone pain and MM diagnosis was 220 days. Regardless of recorded bone pain, laboratory investigations for hypercalcaemia, renal impairment, and anaemia and were conducted in 36.4%, 74.2%, 65.6% and of patients prior to MM diagnosis, respectively. Approximately 5.5% of patients presented with hypercalcemia, 13.5% with renal impairment and 31.3% with anemia. The median time from the first-recorded hypercalcaemia, renal impairment or anaemia event to MM diagnosis was 23, 58 and 73 days, respectively. An imaging investigation or referral for an imaging investigation was recorded for approximately 60% of patients with bone pain/SRE and 32% without bone pain/SRE. One out of five patients with bone pain/SRE and imaging investigations had a record of magnetic resonance imaging or computed tomography scan (Table 1).
Conclusions: Nearly half of patients with newly diagnosed MM presented with a bone pain symptom in primary care, approximately 7 months prior to MM diagnosis. Investigations for hypercalcaemia were not frequent in patients presenting with bone pain, and tests to explore CRAB criteria were underutilized. Underuse of targeted imaging in patients presenting with bone pain was observed. Early recognition and testing for clinical features of MM in primary care may potentially expedite the disease diagnosis and lead to timely medical care.
Seesaghur:Amgen (Europe) GmbH: Current Employment, Current equity holder in publicly-traded company. Petruski-Ivleva:Aetion: Current equity holder in private company, Ended employment in the past 24 months. Banks:Amgen (Europe) GmbH: Ended employment in the past 24 months, Other: Contract worker at Amgen during the conduct of the study. Wang:Aetion: Current Employment, Current equity holder in private company. Mattox:Aetion: Current Employment, Current equity holder in private company. Abbasi:Amgen (Europe) GmbH: Other: Contract worker at Amgen. Maskell:Amgen (Europe) GmbH: Current Employment, Current equity holder in publicly-traded company. Neasham:Amgen (Europe) GmbH: Current Employment, Current equity holder in publicly-traded company. Ramasamy:Takeda: Honoraria; Janssen: Honoraria; Janssen: Research Funding; Takeda: Research Funding; Sanofi: Honoraria; Amgen: Research Funding; Janssen: Membership on an entity's Board of Directors or advisory committees; Abbvie: Membership on an entity's Board of Directors or advisory committees; Amgen: Membership on an entity's Board of Directors or advisory committees; Takeda: Membership on an entity's Board of Directors or advisory committees; Bristol Myers Squibb: Honoraria; Oncopeptides: Honoraria; Takeda: Speakers Bureau; Bristol Myers squibb: Membership on an entity's Board of Directors or advisory committees; Bristol Myers Squibb: Research Funding; Amgen: Honoraria; GSK: Membership on an entity's Board of Directors or advisory committees; Sanofi: Membership on an entity's Board of Directors or advisory committees; Oncopeptides: Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal